3DKnee™ System
3DKnee™ System
Active Confidence in Every Step.
The 3DKnee is a premium high flexion total knee replacement designed after a decade of research. The 3DKnee instills confidence through every step of the total knee replacement process, from the surgeon’s joint selection decision, to the surgical procedure and patient post-operative function.
Confidence in Design
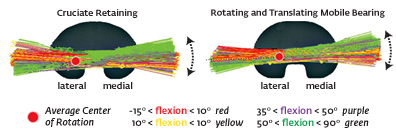
Over a decade of research confirmed that the ACL deficient total knee has very different kinematics from an ACL intact normal knee.1,2 The 3DKnee is based on data from insert retrievals, tibial plateau analysis, and fluoroscopic review (shown in Figures A and B) which concluded that an ACL deficient knee has a lateral rotational bias. With a ball and socket lateral condyle for rotation and a flatter medial condyle designed for translation, the 3DKnee is designed to allow ACL deficient TKA kinematics. The design has performed successfully in vivo with excellent Knee Society scores.3
Confidence in Procedure
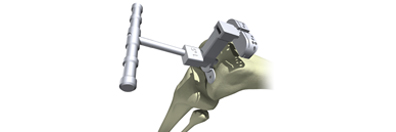
Through every step of the 3DKnee procedure, surgeons have accurate guidance from the instrumentation and yet are allowed the freedom and flexibility to alter intra-operative plans as needed. M.I.K.A.™ (minimally invasive knee arthroplasty) or standard incision instruments are available and allow a surgeon to work confidently through the best incision possible for each patient.
Confidence in Motion
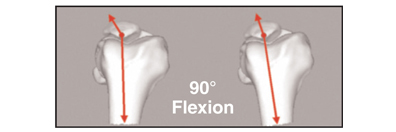
As most knee replacement patients reach maximum flexion when femoro-tibial impingement occurs, the 3DKnee insert sulcus is positioned 5mm posterior to the AP center, encouraging roll-back and delaying ROM-limiting impingement.1 A posterior based technique allows for maintenance of the posterior condylar offset of the femur.2 While a single radius of curvature allows 1:1 contact through mid-flexion, control of translation is relaxed as the knee goes into deeper flexion, allowing ligamentous structures to take control.

Confidence in Strength
A very congruent, stable articulating surface allows for the quadriceps muscles to operate much more efficiently, reducing hamstrings co-activation and the demands on the extensor mechanism, making patients effectively stronger as a result of an intrinsically stable knee joint.1,3,4,7,8
Confidence in Stability
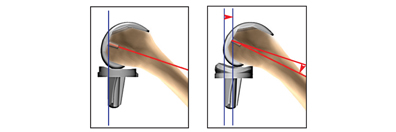
By controlling the translation of the lateral condyle in extension, and giving increased lateral A/P laxity in flexion, the 3DKnee articulating surface is designed to accommodate for the loss of the ACL and provide intrinsic AP stability to the replaced knee.4 The 3DKnee femoral design incorporates a single radius of curvature. This design feature seeks to reduce mid-flexion instability and creates a more stable joint in terms of varus/valgus laxity.5,6 Less compensatory muscle activity is required to stabilize the total joint.7 The 3DKnee insert is used with or without an intact PCL. A stable articulating surface is created without the use of a less bone sparing post and cam design. The high anterior lip and conforming articulating surface stabilize the femur on the insert.
- Videos
- Features & Benefits
- Components
- Links
- References

3DKnee Patient Testimonial

Surgical Knee Animation
Walt's Ride - Surgical Knee Patient Testimonial
Enhances Quadriceps Function
Provides excellent power, especially early in flexion, by rolling out to engage the patella quickly, while maintaining great leverage by preventing anterior slide and shortening of the quadriceps lever-arm. Rollout of the femur aligns the quadriceps to the center of the patella, improving quadriceps leverage while reducing patella stresses.
Improves Fermoral/Patella Mechanics
Improves femoral-patella mechanics by promoting early rollout of the femur to engage the patella in a deep patella groove.
Improves ROM
Improves range of motion by maintaining the posterior position of the femoral condyles on the tibia during flexion.

Reduces Contact Stress
Increases implant longevity by reducing polyethylene contact stresses as a result of a congruent lateral condyle.
Tibial Component
- Asymmetric baseplate
- Winged keeled geometry
- Two tibia size options for each 3DKnee insert
Femoral Component
- Congruent lateral condyle
- Deepened and lateralized patella groove
- Wide medial condyle
- Constant axis curvature for increased contact area up to 80°
Insert
- Direct Compression Molded or e+™ options
- Congruent lateral condyle
- Size specific for optimal congruency to the femur
- Centered posteriorly to encourage increased femoral rollback
- Wide medial condyle to reduce contact stresses
Domed Patella
- Domed Geometry for optimal contact area with the deepened trochlear groove
- Available in sizes 26-38mm
These links will take you to non-DJO Surgical web sites to which this site's Legal Policy does not apply. You are solely responsible for your interactions with these sites.
Popular Science Article: Will We Merge with Machines?
AAOS
- Banks, S.A., Harman, M.K., Bellemans, J., Hodge, W.A.: Making Sense of Knee Arthroplasty: News You Can Use. The Journal of Bone and Joint Surgery. 2003; 85:64-72.
- Bellemans, J., Bansk, S.A., Victor, J., Vandenneucker, H., Moemans, A.: Fluoroscopic Analysis of the Kinematics of Deep Flexion in Total Knee Arthoplasty: Influence of Posterior Condylar Offset. The Journal of Bone and Joint Surgery, Vol. 84-B, No. 1, January 2002.
- Hodge, W.A., Banks, S.A., Mitchell, K.: Early Clinical Gait Laboratory and Fluoroscopic Experience with the 3DKnee Total Knee Arthroplasty. White Paper, The Hodge BioMotion Foundation, West Palm Beach, FL. 2004.
- Banks SA, et al.: Does Intrinsic Stability Provide Enhanced Ability in PCL Retaining TKA? Proc Orthop Res Soc, 2004.
- Wang H., Simpson K.J., Ferrara M.S., Chamnongkich S., Kinsey T., Mahoney O.M.: Biomechanical differences exhibited during sit-to stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006 Dec;21(8):1193-9.
- Kessler O, Dürselen L, Banks S, Mannel H, Marin F.: Sagittal curvature of total knee replacements predicts in vivo kinematics. Clin Biomech (Bristol, Avon). 2007 Jan;22(1):52-8. Epub 2006 Oct 9.
- Mahoney OM, McClung CD, dela Rosa MA, Schmalzried TP.: The effect of total knee arthroplasty design on extensor mechanism function. J Arthroplasty. 2002 Jun;17(4):416-21.
- Mitchell, K., Banks, S.A., Rawlings, J., Wood, S.A., Hodge, W.A.: Strength of Intrinsically Stable TKR during Stair Climbing. White Paper, The Hodge BioMotion Foundation, West Palm Beach, FL. 2004.
- Harman, M.K., Markovich, G.D., Banks, S.A., Hodge, W.A.: Wear Patterns on Tibial Plateaus From Varus and Valgus Osteoarthritic Knees. Clinical Orthopaedics and Related Research, No. 352, July 1998.
- Ginsel BL, Banks S, Verdonschot N, Hodge WA. Improving maximum flexion with a posterior cruciate retaining total knee arthroplasty: a fluoroscopic study. Acta Orthop Belg. 2009 Dec;75(6):801-7.
- Mikashima Y, Tomatsu T, Horikoshi M, Nakatani T, Saito S, Momohara S, Banks SA. In vivo deep-flexion kinematics in patients with posterior-cruciate retaining and anterior-cruciate substituting total knee arthroplasty. Clin Biomech (Bristol, Avon). 2010 Jan;25(1):83-7.
- DesJardins J. Wear Testing Simulation Performance and Outcomes for 3DKneeTM Total Knee Prosthesis. White paper, Clemson University Department of Bioengineering.
- Morra EA, Greenwald AS. High Flexion in Contemporary Total Knee Design: A Precursor of UHMWPE Damage? A finite element study. AAOS 2007: 2007 Orthopaedic Research Laboratories, Cleveland, Ohio.